Background:
Effective communication within a healthcare team leads to improved patient safety, more effective interventions, enhanced employee morale, and increased patient and family satisfaction. Our study aims to improve interprofessional communication between hematologists and referring providers in our ambulatory hematology clinic. First, we assessed the frequency with which hematologists communicated patient care recommendations to referring providers. After we identified a gap in communication, we implemented a quality improvement intervention to address the gap.
Methods:
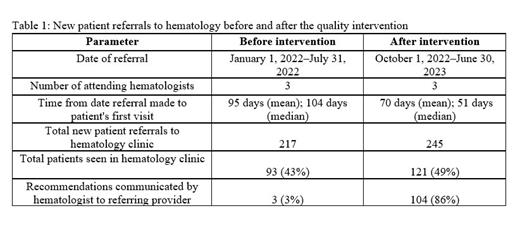
A retrospective review was conducted to identify new patients ≥18 years old referred to the hematology clinic from January 1, 2022, to July 31, 2022. The data assessed included demographics, reason for referral, show rate, time from referral to first visit, and whether there was documentation of recommendations communicated from the hematologist to the referring provider. Communication was also counted if the patient was referred from an internal provider who had access to the medical record. After a gap in communication was identified, we implemented a quality improvement measure to document referring providers' names and contact information in every initial office visit note and then fax over all new patient notes with hematology recommendations to the referring provider at the end of each week. All fax communications were documented in patients' electronic charts.
Results:
A total of 217 new patients were referred to the hematology clinic from January 1, 2022, to July 31, 2022. The median age was 53 (range, 18-94) years; 43% of patients were seen in the clinic, and 56% were no-shows. Primary referral reasons were anemia (44%), thrombosis (21%), leukocyte abnormalities (12%), and thrombocytopenia (11%). The average time between referral date and first visit was 95 days. Of the 43% (n=93) of patients seen in the clinic, only 3% (n=3) had documented communication between the hematologist and referring provider prior to the quality intervention. In the second phase of the study, data was collected after implementation of the intervention from October 1, 2022, to June 30, 2023. There were 245 new patient referrals, with 49% of patients seen in clinic. The average time between referral date and first visit was 70 days. The rate of communication between the referring provider and hematologist improved to 86%.
Conclusion:
At our outpatient hematology clinic, we identified a gap in communication between the referring providers and hematologists. Often a provider refers a patient to hematology but is unaware of the recommendations that were made. This can lead to unclear recommendations and treatment plans, poor patient care, and frustration among patients and providers. We implemented an intervention to improve communication with referring providers. Our intervention was successful in improving the communication flow and enhanced communication from 3% to 86%. We recommend adoption of our intervention by other clinics at our institution to enhance their communication flow between referring providers and specialists. Our study identified additional issues, including a high no-show rate and long wait time from referral date to first visit. Although this was not the primary focus of our quality improvement project, additional quality improvement measures aimed at addressing these gaps are needed.
Disclosures
Idowu:Bluebird Bio: Consultancy; Forma Therapeutics: Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding, Speakers Bureau; Novo Nordisk: Consultancy, Research Funding; Vertex: Consultancy; Global Blood Therapeutics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Alexion: Research Funding; Agios Pharmaceuticals, Inc.: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal